Trauma and Sleep: Why PTSD and Insomnia Often Go Hand in Hand
Trauma and Sleep: Why PTSD and Insomnia Often Go Hand in Hand
Trauma and sleep disturbances feed into each other in a vicious cycle. Whereby, the brain and body stay in a hypervigilant state post-trauma, it makes it difficult to relax enough to fall asleep. Such a state of arousal marked by increased heart rate, racing thoughts, and always being wound up prevents the body from entering restorative sleep stages. Nightmares and flashbacks exacerbate the inability to sleep well, leading to frequent awakenings and further engraining a fear of sleeping. This gradually transforms into chronic insomnia, where a conditioned brain fails to associate time for sleep as rest but stress, making it even more impossible to break from the cycle.
Poor sleep results in more effects than just an overwhelming feeling of tiredness. Inadequate sleep impairs emotional regulation, weakens memory processing, and increases stress hormones like cortisol, all of which worsen the symptoms of PTSD. Sleep deprivation also reduces the brain’s ability to process traumatic memories properly, keeping them stuck in an unprocessed, intrusive state. This means that while PTSD disrupts sleep, the lack of sleep, in turn, intensifies PTSD symptoms, creating a self-perpetuating loop.
Both conditions must be treated simultaneously, either with cognitive behavioral therapy for insomnia (CBT-I), trauma-focused therapy, medication, or relaxation techniques. The improvement in sleep quality can lead to better control of symptoms and, therefore, a more realistic recovery.
What is Insomnia?
Insomnia is not just a couple of sleepless nights; it is a continuous disruption of the body’s ability to rest, recover, and reset. It is the racing mind when the world is silent, the tired body unable to surrender to sleep. Insomnia is not just about failing to fall asleep but also waking up too often, too early, or feeling completely unrested after spending hours in bed. This deprivation gradually leads to the wear and tear not only on mental but also on physical health by causing mood swings, failing concentration, weakened immunity, and a highly heightened stress response. Whether caused by stress, anxiety, trauma, or perhaps lifestyle habits, insomnia can easily become a frustrating cycle where the more one tries to sleep, the more elusive it becomes.

Causes of Insomnia:
Other conditions leading to sleeplessness are attributed to multiple underlying psychological, physiological, and environmental factors. Such include some of the common underlying reasons for suffering from insomnia explained below.
a. Stress and Anxiety
Racing thoughts, anxiety, and hyperactive mind can really make sleeping time non-existent. Work stress, financial tensions, failing relationships, or other life-altering changes can often be a cause of insomnia. Even more common causes include generalized anxiety and PTSD as generalized anxiety keeps the nervous system constantly on the edge, hence sleep eludes it.
b. Poor Sleep Habits
Irregular sleep schedules, bingeing on screen time before bed, drinking caffeine or alcohol close to bedtime, and stimulating events before sleep will all interfere with the body’s overall natural wake-sleep cycle. That is, an irregular bedtime schedule can mess up the body’s internal clock to make it difficult to fall asleep or remain asleep.
c. Medical Conditions and Medications
Chronic pain, acid reflux, asthma, heart disease, and neurological disorders are also factors that disrupt sleep. Some prescriptions, such as antidepressants, stimulants, and blood pressure medication, may also cause insomnia due to side effects.
d. Hormonal Changes
Changes in hormones—like when a woman is pregnant, experiencing menopause, or has a thyroid disorder—affect the way individuals sleep. Shifts in melatonin and cortisol hormone can also disrupt the body’s internal rhythm.
e. Mental Health Disorders
Depression, PTSD, and other mental health conditions can significantly disrupt sleep patterns. While some individuals experience excessive sleep, others struggle with persistent insomnia, creating a feedback loop that worsens both sleep and mental health.
Understanding the root cause of insomnia can help find a proper treatment. Whether it’s stress, better sleep hygiene, or management of an underlying medical condition, targeting insomnia at its root can allow for restful sleep to be regained.
Understanding PTSD
Post-Traumatic Stress Disorder, or PTSD, is an anxiety disorder related to a frightening experience or threat of death that causes significant psychological distress. Its symptoms are often more than just a normal reaction to stress: they are something that leaves someone stuck in the heightened state of fear, anxiety, or emotional distress long after the danger is gone. There are various life-threatening experiences including accidents, natural disasters, being exposed to war, assault, abuse, among others.
The common symptoms of intrusive are flashbacks, nightmares, and distressing memories that cause them to relive the trauma. They also tend to exhibit avoidance behaviors by avoiding places, people, or situations that remind them of the event. Other changes in mood and cognition that can be attributed to PTSD include feelings of detachment, guilt, or emotional numbness. Notable symptoms include hyperarousal, often manifesting as irritable mood, difficulty concentrating, insomnia, and exaggerated startle response. These symptoms keep the nervous system in a chronic state of alertness, which makes it hard to relax.
PTSD can severely interfere with daily life, relationships, and well-being, but proper treatment, such as therapy, medication, and coping skills, can help work towards recovery and regaining some control over life.

Symptoms of PTSD
The symptoms can be severe in intensity and manifest shortly after a traumatic event, or even several years later. They are grouped into four basic categories: intrusion, avoidance, negative changes in mood and cognition, and hyperarousal.
a. Intrusive Symptoms
- Flashbacks – The victim feels that he or she is reliving the traumatic event again.
- Nightmares – Distressing dreams about the trauma.
- Forced Recollection – Recurrent and distressing thoughts about the event.
- Emotional and Physical Reactions -The person suffers from intense emotional distress or even more physical symptoms, such as a fast heartbeat or sweating, whenever they are reminded of the trauma.
b. Avoidance Symptoms
- Avoided places, people, or activities – Avoiding anything that may trigger memories of the trauma.
- Emotional numbing – Unable to experience joy or love.
- Inhibiting thoughts and emotions – Avoiding conversations or reminders about the trauma.
c. Negative Changes in Mood and Cognition
- Persistent Negative Thoughts – Hopelessness, self-guilt, or self-blame
- Memory Problems – Failure to recall a crucial element of the traumatic experience.
- Loss of Interest – Loss of interest in activities which a person would have earlier found pleasurable.
- Social Withdrawal – Strong isolation, and feeling cut off from others.
How trauma affects sleep?
Trauma causes a lot of effects on the brain and the body, mostly in terms of how they deal with stress and relaxation. As a result of a disturbing incident, for example, military combat, abuse, natural disasters, or accidents; the brain will have developed hyperactivity of threat-detection in the brain’s system. An overactive amygdala manages the body’s fight-or-flight response.
It can cause in an overactivated system the following:
- Hyperarousal which makes one cannot relax and therefore sleep.
- Inability to reach deep sleep, which will prevent full-body rest and recovery.
- Increased levels of stress hormones, such as cortisol, disrupt the sleep cycles.
- Frequent wakings because of nightmares or intrusive memories.
The Relationship Between PTSD and Insomnia
PTSD and insomnia are deeply connected, creating a cycle where trauma disrupts sleep, and sleep deprivation worsens PTSD symptoms. People with PTSD often struggle with nightmares, racing thoughts, and heightened anxiety, making it difficult to fall or stay asleep. At the same time, lack of restful sleep impairs emotional regulation and increases stress, making PTSD symptoms even more intense. Understanding this relationship is crucial for finding effective treatments that address both conditions together.
1. Hyperarousal and Sleep Disturbances
Hyperarousal is one of the hallmarks of PTSD, leaving the body at a heightened level of alertness. This level of alertness makes it impossible for people to fall asleep or stay asleep as their nervous system remains in an alert state of expecting danger.
Hyperarousal can cause:
- Sleep onset insomnia: a person finds it hard to fall asleep.
- Waking up repeatedly at night (sleep maintenance insomnia)
- Waking up from sleep after hours, yet still feeling really tired
2. Nightmares and Flashbacks
In the case of individuals with PTSD, sleep is frequently disrupted by nightmares and flashbacks associated with their trauma. These nightmares can make people wake up in a panic, drenched in sweat, or feeling like they are reliving their trauma. This, over time, can lead to fear of sleep, causing the sufferer to actively avoid going to bed and exacerbating insomnia.
3. Altered Sleep Architecture
Research has shown that PTSD interrupts sleep patterns, especially REM sleep; REM sleep is an essential stage for emotional processing. People suffering from PTSD have:
- REM sleep: It’s shortened to result in emotional regulation.
- Frequent awakenings during REM, meaning continuous distressing.
- Decreased deep sleep impacts recovery of the body, and cognition.
4. Comorbid Mental Illnesses
PTSD rarely occurs alone—it is often accompanied by anxiety, depression, and substance use disorders, all of which can contribute to insomnia. Anxiety leads to rumination and racing thoughts, while depression is linked to early morning awakenings and fragmented sleep.

The Long-Term Effects of PTSD-Related Insomnia
Chronic sleep disturbances can have serious consequences on physical and mental health. Those with PTSD-related insomnia are at higher risk for:
- Worsening PTSD symptoms, making trauma harder to process.
- Increased risk of cardiovascular diseases due to prolonged stress.
- Weakened immune function, leading to frequent illness.
- Cognitive decline, affecting memory, focus, and decision-making.
- Substance abuse, as individuals may turn to alcohol or drugs to cope with sleeplessness.
This cycle of poor sleep and heightened stress can make PTSD symptoms more severe and long-lasting, which is why addressing sleep issues is crucial for recovery.
Effective Strategies for Managing PTSD-Related Insomnia
PTSD-related insomnia can be challenging, but there are several treatments and coping strategies that can help improve sleep quality.
1. Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT-I is the gold standard for treating insomnia, especially in patients with PTSD. It includes:
- Challenging negative beliefs about sleep
- Establishing a consistent bedtime routine
- Using relaxation techniques to calm the nervous system
- Practicing stimulus control, such as using the bed only for sleep
2. Exposure Therapy for PTSD Nightmares
For those whose nightmares are especially severe, IRT can be very helpful. This includes:
- Rewriting the nightmare with a positive or neutral ending
- Practicing the new dream scenario while awake
- Gradually reducing the fear associated with sleep
3. Medication Options
While therapy should always be the first line of treatment, some people benefit from medications such as:
- Prazosin, which helps reduce PTSD-related nightmares
- Melatonin: a natural sleep aid, controls the sleep-wake cycle
- Antidepressants: sometimes for co-occurring anxiety and depression
But medications must only be used when prescribed by a doctor since certain sleeping pills might worsen the symptoms after a period of time.
4. Lifestyle Changes to Improve Sleep Quality
Even lifestyle changes can contribute much to improve the quality of sleep:
- Restrictive use of caffeine and alcohol since both can disrupt the sleep cycle.
- Developing a soothing bedtime routine, such as meditation or deep breathing.
- Regular exercise, but not intense exercise before bedtime.
- Blackout curtains and white noise machines can create an ideal sleep environment.
5. Mindfulness and Relaxation Techniques
Mindfulness, yoga, or progressive muscle relaxation can help calm nighttime anxiety and lead to better sleep. These techniques teach the brain to focus on the present rather than dwelling on past trauma.
Final Thoughts
PTSD is closely related to insomnia, whereby trauma usually leads to chronic sleep disturbances that result in aggravation of the state both mentally and physically. However, one can break this cycle by combining the perfect blend of therapy and lifestyle changes with self-care to regain good sleeping habits.
If you or someone you know is struggling with PTSD-related insomnia, seeking professional help can be a life-changing step toward recovery. Sleep is not just a luxury—it is a crucial part of healing, and everyone deserves the opportunity to rest peacefully.
Have you experienced PTSD-related sleep problems? Share your thoughts and experiences in the comments below, and help raise awareness about the impact of trauma on sleep!

Obsessive-Compulsive Disorder (OCD) and Anxiety: Are They Connected?
Obsessive-Compulsive Disorder (OCD) and Anxiety: Are They Connected?
Obsessive-Compulsive Disorder (OCD) and anxiety are often mentioned in the same breath, and for good reason. Both conditions can be overwhelming, affecting daily life, thoughts, and behaviors. But what exactly is the connection between OCD and anxiety? Are they the same thing, or are they distinct disorders with overlapping symptoms?
It is a natural response to feeling anxious or threatened. It can take different forms-excessive worry, restlessness, and racing heart, sweating, or shortness of breath-though anxiety disorders are not in themselves diagnosable medical conditions. An anxiety disorder, rather, is a disorder of excessive worry that is disruptive and pervasive, not just occasional.
OCD, on the other hand, involves persistent, intrusive thoughts called obsessions. These create distress and lead to compulsive behaviors that are meant to reduce that distress. Unlike generalized anxiety that often arises from real-life concerns, OCDs tend to be more irrational and exaggerated, which makes them harder to control.
Despite their differences, OCD and anxiety disorders share many similarities, including their neurological basis, treatment methods, and the emotional toll they take on those affected. Understanding the link between them can help individuals seek the right treatment and support.
Understanding Anxiety
Anxiety is a natural response when the brain detects a potential danger. It acts as a survival mechanism that assists in the fight against danger through increased alertness, heart rate, and adrenaline levels. When anxiety becomes too much, persists, or is uncontrollable, it interferes with daily life and leads to an anxiety disorder.
There are several types of anxiety disorders, including:
a. Generalized Anxiety Disorder (GAD): Persistent worry about various things in life, including work, health, or relationships.
b. Panic Disorder: Sudden and recurring episodes of intense fear, often considered to have physical manifestations, for example chest pain, dizziness, or shortness of breath.
c. Social Anxiety Disorder: Extreme fear of social interactions and situations with avoidance behavior.
d. Phobias: Intense fear of specific objects or situations, such as heights, flying, or enclosed spaces.

Common symptoms of anxiety include:
- Worry or fear that is persistent
- Difficulty concentrating
- Sleep disturbances
- Muscle tension and fatigue
- Rapid heartbeat and difficulty breathing
- Irritability and restlessness
When anxiety becomes chronic, it can severely impact mental and physical well-being. Understanding anxiety and its symptoms is crucial in seeking appropriate treatment and support.
What is OCD?
Obsessive-Compulsive Disorder (OCD) is a chronic mental health condition characterized by two main components: obsessions and compulsions.
Obsessions are intrusive, unwanted thoughts, images, or urges that produce distress or anxiety. Such obsessions may center on fear of contamination, causing harm, or symmetry and cannot be easily suppressed.
Compulsions are compulsive, repeated behaviors or mental rituals intended to reduce the anxiety associated with obsession. Such actions may involve overcleaning, checking, counting, or repetition of phrases.
Unlike general anxiety, which is often based on real-life stressors, OCD thoughts are usually irrational and exaggerated. However, the individual feels compelled to act on them to relieve distress, creating a vicious cycle of obsessive thinking and compulsive behaviors.
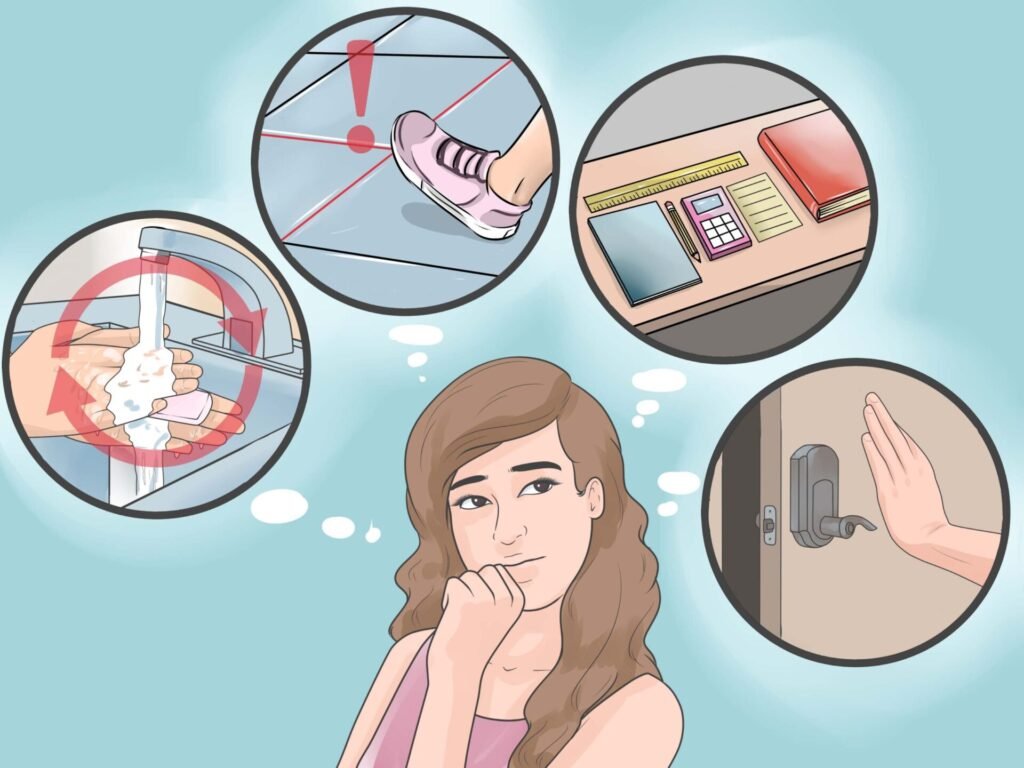
Some common examples of OCD symptoms include:
a. Repeatedly washing hands or sanitizing due to fear of germs.
b. Checking doors, locks, or appliances multiple times to prevent harm.
c. Rearranging objects in an “exact” way for things to feel “just so”.
d. Repeating prayers, words, or numbers in one’s mind to prevent “bad” things
from happening.
OCD can be very debilitating and time consuming and disrupt daily life,
work, and personal relationships. Knowing the symptoms and getting the proper
treatment is necessary to help manage the disorder.
The Relationship of OCD to Anxiety
Obsessive-Compulsive Disorder (OCD) is closely linked to anxiety, as it is driven by intrusive thoughts (obsessions) that cause distress and lead to repetitive behaviors (compulsions) aimed at reducing that anxiety. While anxiety disorders involve excessive worry and fear, OCD manifests through ritualistic actions intended to relieve uncertainty and discomfort. Both conditions share overlapping symptoms, including heightened stress responses and difficulty controlling anxious thoughts. Effective treatments, such as cognitive-behavioral therapy (CBT) and medication, target these underlying anxieties to help manage OCD symptoms.
1. OCD was Once Labeled as an Anxiety Disorder
Obsessive-compulsive disorder was also thought to be an anxiety disorder because the stress from obsessions is very severe and leads to a high anxiety level. Recently, however, OCD was included in its category: Obsessive-Compulsive and Related Disorders, which is part of the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition). Although its classification has been changed, OCD is still somehow related to anxiety.
2. Anxiety Drives OCD Behaviors
OCD subjects experience severe anxiety caused by obsessions. The only way they can reduce such anxiety is by performing compulsive acts. Such acts may momentarily reduce the level of anxiety, but they only perpetuate the obsessive-compulsive cycle, worsening the anxiety.
3. Analogous Brain Activity in Anxiety and OCD
Neuroscientific research has shown that both OCD and anxiety disorders involve overactivity in brain regions responsible for fear processing and emotional regulation, particularly the amygdala, prefrontal cortex, and basal ganglia. This neurological overlap suggests a deep connection between the two conditions.
4. Co-Occurrence is Common
It’s not uncommon for a person with OCD to also have another anxiety disorder. Studies have shown that 75% of those who suffer from OCD have had some time in their lives experiencing generalized anxiety disorder, panic disorder, or social anxiety disorder.
Differences Between OCD vs Generalized Anxiety
Even though OCD and anxiety disorders have much in common, they also differ in other areas:
a. Obsessions vs. General Worries: Anxiety disorders include persistent worries about real-life issues (e.g., finances, work, relationships), whereas OCD includes irrational, intrusive thoughts that feel uncontrollable.
b. Compulsions vs. Avoidance: In anxiety disorders, people tend to avoid stressors (e.g., avoidance of social situations in social anxiety disorder). In OCD, people feel compelled to perform ritualistic behaviors to neutralize distress.
c. Sense of Control: Individuals with OCD realize how nonsensical their thoughts and behaviors are but feel unable to halt them, putting them outside normal experience. People with anxiety disorders tend to believe that their fears are more realistic.
Treatment for OCD and Anxiety
Fortunately, both OCD and anxiety disorders are treatable. Common treatment approaches include:
1. Cognitive-Behavioral Therapy (CBT)
The key benefit of CBT is helping patients overcome their negative thought patterns. Exposure and Response Prevention, a form of CBT, is also known to be helpful in OCD, where it slowly exposes patients to their fears but prevents the urge to do the compulsive behaviors.
2. Medication
SSRIs such as fluoxetine, sertraline, and fluvoxamine are the commonly used medications for OCD and anxiety disorders. SSRIs work on increasing serotonin levels in the brain that eventually leads to the decrease of symptoms.
3. Mindfulness and Stress-Reduction Techniques
Mindfulness, deep breathing, and meditation can help individuals control anxiety and prevent compulsions by making them more aware and in control.
4. Lifestyle Changes
Exercise, a healthy diet, and adequate sleep are crucial in reducing symptoms of OCD and anxiety. Caffeine and alcohol should be avoided to stabilize mood and anxiety levels.
Final Thoughts
While OCD and anxiety disorders are separate conditions, they are highly interrelated. Anxiety is central to the maintenance of OCD symptoms, and most people have both conditions at the same time. A better understanding of these conditions can lead to better quality of life through proper treatment.
If you or someone you know suffers from OCD or anxiety, consulting a mental health professional is the best step toward managing symptoms and regaining control. With the right support, coping strategies, and treatment, it is possible to lead a fulfilling and balanced life despite these challenges.
