Understanding the Different Types of Depression: Major Depressive Disorder, Dysthymia, and Bipolar Disorder
Understanding the Different Types of Depression
Depression is a complex mental health condition that affects millions of people worldwide, but it’s not a one-size-fits-all disorder. Many people think of depression as simply feeling sad, but the reality is far more nuanced. It manifests in various forms, each with its own set of symptoms, causes, and treatment options. Understanding these different types of depression is crucial for recognizing the signs and seeking the appropriate help.
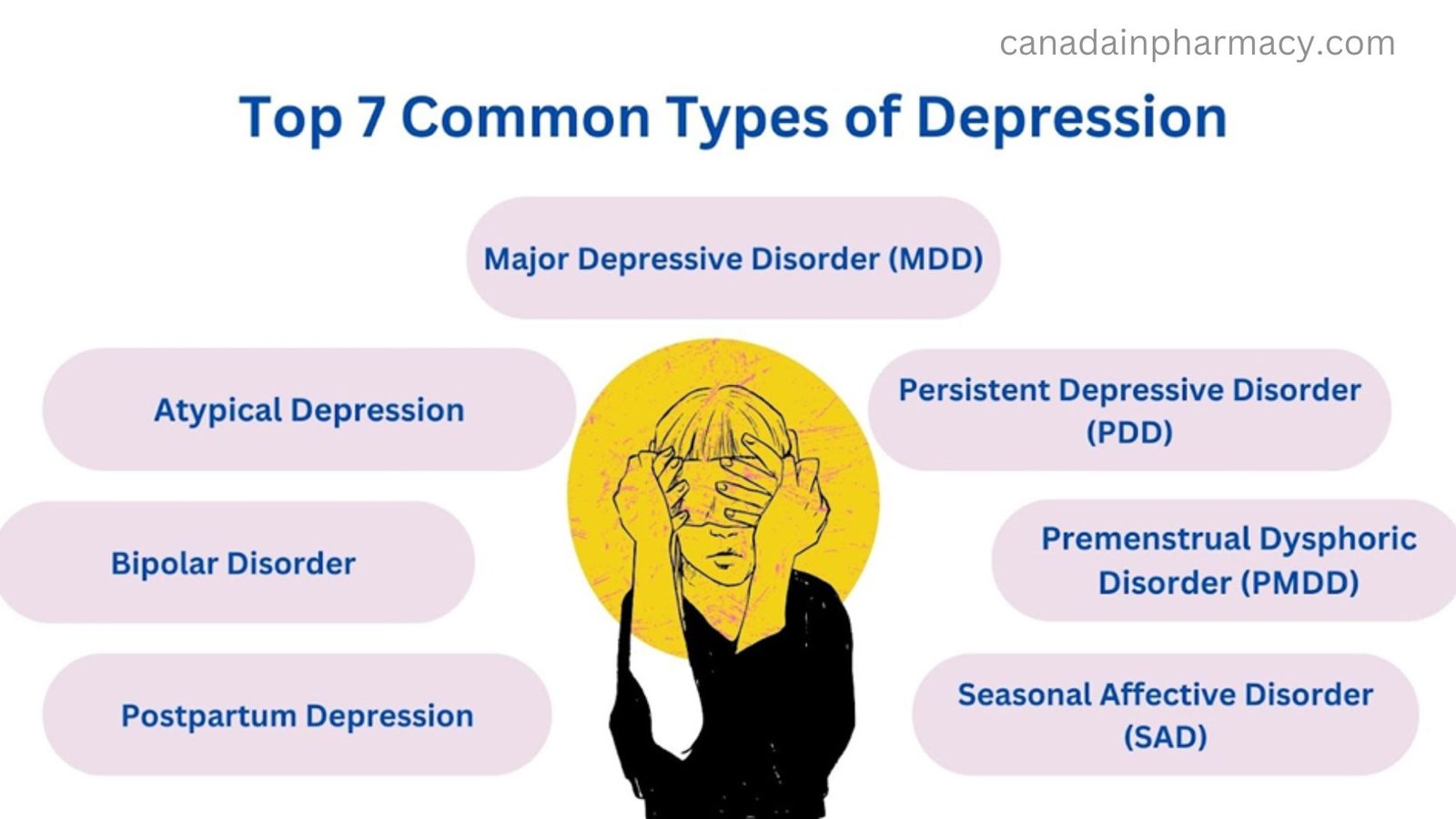
From Major Depressive Disorder (MDD), which is the most common form, to more specific types like Seasonal Affective Disorder (SAD) and Postpartum Depression (PPD), each type can impact a person’s life in unique ways. The key to managing depression lies in identifying which form it takes and tailoring the treatment accordingly.
This blog aims to break down the different types of depression, explore their symptoms, and provide insights into how they can be treated. Whether you or someone you know is affected, understanding the distinctions between these conditions can pave the way for effective support and healing.
Causes of Depression
It is a multifactorial condition, meaning its causes are often complex and vary from person to person. Several factors can contribute to the onset, and they may interact in different ways. Here are some of the main causes:
1. Biological Factors
- Genetics: A family history of depression or other mental health disorders can increase the risk of developing depression. Certain genetic traits may make individuals more susceptible to the condition.
- Brain Chemistry: Neurotransmitters, such as serotonin, norepinephrine, and dopamine, play a key role in regulating mood. Imbalances in these chemicals can contribute to feelings of depression.
- Hormonal Changes: Hormonal shifts, such as those occurring during pregnancy, the postpartum period, menopause, or thyroid imbalances, can trigger or worsen depression.
2. Psychological Factors
- Chronic Stress: Ongoing stress from work, relationships, or financial issues can overwhelm a person’s ability to cope, leading to depression.
- Trauma or Abuse: Past traumatic experiences, especially during childhood, can significantly impact mental health and increase the risk of depression. This includes physical, emotional, or sexual abuse, as well as witnessing violence.
- Low Self-Esteem: People with negative self-perceptions and a lack of confidence may be more vulnerable to developing depression, particularly in response to failure or setbacks.
3. Environmental Factors
- Social Isolation: Lack of support from friends, family, or community can contribute to loneliness, which is a risk factor for depression.
- Major Life Changes: Significant life events, such as the death of a loved one, divorce, job loss, or moving to a new place, can lead to feelings of sadness and helplessness that may evolve into depression.
- Living Conditions: Living in poverty, facing discrimination, or experiencing unstable housing can increase stress and reduce access to the resources needed to maintain mental health.
4. Medical Conditions
- Chronic Illnesses: People with long-term health problems, such as diabetes, heart disease, cancer, or chronic pain, may experience depression as a result of the physical and emotional burden these conditions impose.
- Medications: Certain medications, especially those used to treat other medical conditions, can have side effects that contribute to depression.
- Sleep Disorders: Poor sleep or conditions like insomnia can exacerbate depression or even contribute to its development.
5. Substance Abuse
- Drug or Alcohol Use: Substance abuse can lead to or worsen depression. Drugs and alcohol can disrupt brain function and alter mood, leading to a cycle of depression and substance dependence.
6. Social and Cultural Factors
- Cultural Expectations: In some cultures, there may be pressure to conform to societal norms or expectations, which can lead to feelings of inadequacy or depression if one feels they do not meet those standards.
- Stigma: The stigma surrounding mental health, particularly depression, can prevent individuals from seeking help, allowing the condition to worsen over time.

Different Types of Depression
1. Major Depressive Disorder (MDD)
What is it? Major Depressive Disorder, also referred to as clinical depression, is the most common diagnosed. It is characterized by persistent feelings of sadness, hopelessness and seeming emptiness, and lack of interest in activities that were pleasurable. The symptoms can be disabling and interfere with several daily functioning tasks.
Symptoms:
- Persistent feeling of sadness or “empty” mood
- Loss of interest or pleasure in activities once enjoyed
- Fatigue or lack of energy
- Difficulty concentrating or making decisions
- Changes in appetite (either weight loss or gain)
- Sleep disturbances (insomnia or excessive sleeping)
- Thoughts of death or suicide
Treatment:
- Antidepressant medications (SSRIs, SNRIs)
- Cognitive Behavioral Therapy (CBT)
- Lifestyle changes (exercise, diet, and sleep improvements)
2. Persistent Depressive Disorder (PDD)
It refers to Persistent Depressive Disorder. This is known as dysthymia formerly, the symptoms of which last for two years or longer. Though they are somewhat different than that experienced in MDD, symptoms for PDD generally less severe but persistent. Individuals affected by PDD often experience most of their life with feelings of “low” and loss of energy or low self-esteem.
Symptoms:
- Longstanding feelings of hopelessness
- Low self-esteem and motivational behaviors
- Feelings of helplessness
- Poor performance at the workplace or interpersonal relationships
- Insomnia or sleep disturbances
Therapy:
- Long-term therapy which includes CBT, Interpersonal Therapy
- Anti-depressant drugs, namely SSRIs, and Tricyclic Antidepressants
- Some lifestyle changes and stress management techniques
3. Bipolar Disorder
What is it? Bipolar Disorder, sometimes called manic-depressive illness, is a serious brain illness that causes an extreme shift in moods. During periods of depression, a person can have low moods (depression) while in other periods of mood elevation they may have emotional highs (mania or hypomania). Manic or hypomanic episodes often accompany depressive episodes of bipolar disorder, characterized by elevated mood, irritability, and impulsive behavior, which differentiate the condition from Major Depressive Disorder.
Depression Symptoms
- Energy is low; fatigability is present.
- Extreme sadness or hopelessness
- Irritability
- Thoughts of death or suicide
- Less interest in activities
Treatment:
- Mood stabilizers (e.g., lithium)
- Antidepressants combined with antipsychotics
- Therapy (CBT, psychoeducation)
4. Seasonal Affective Disorder (SAD)
What is it? Seasonal Affective Disorder (SAD) is a form of depression which usually occurs in the fall and winter months. During these months there is less exposure to natural light. This might affect the inner clock of a person, giving them feelings of sadness, reduced energy, and social withdrawal.
Symptoms:
- Low mood, usually beginning in late fall or early winter
- Low energy and increased sleep
- Weight gain or changes in appetite (craving carbohydrates)
- Social withdrawal and difficulty concentrating
Treatment:
- Light therapy (exposure to a special light box)
- Antidepressants (SSRIs)
- Cognitive Behavioral Therapy (CBT)
- Vitamin D supplements
5. Postpartum Depression (PPD)
What is it? Postpartum Depression is a type of depression that affects many women after childbirth. While some degree of mood swings, known as the “baby blues,” is common after giving birth, postpartum depression is more severe and can interfere with a woman’s ability to care for herself or her baby.
Symptoms:
- Extreme sadness and hopelessness
- Difficulty bonding with the baby
- Intense irritability or mood swings
- Fatigue and changes in sleep patterns
- Suicidal ideas about oneself or the baby
Interventions:
- Antidepressant drugs (SSRIs and SNRIs)
- Psychotherapy (CBT or interpersonal psychotherapy)
- Reassurance of family, friends, or by support groups
6. Atypical Depression
It is a Major Depressive Disorder subtype which is different from typical depression; people with this condition can achieve temporary remission on the symptoms brought about by positive circumstances. However, the symptoms do tend to occur more intensely as things are going sour.
Symptoms:
- Increased appetite or weight gain
- Excessive sleep (hypersomnia)
- Heavy, “lead-like” limbs
- Sensitivity to rejection
- Mood improves temporarily when positive events occur
Treatment:
- Antidepressants (SSRIs, MAOIs)
- Cognitive Behavioral Therapy (CBT)
7. Situational Depression
What is it? Situational depression, which can be more precisely described as adjustment disorder with depressed mood, results from significant life events or situations. Compared with other forms of depression, situational depression often presents as temporary and is correlated with a discrete stressor, including but not limited to job loss, relationship breakup, and the death of an important family member.
Signs and Symptoms
- Sadness
- Feelings of hopelessness
- Dysfunction within life, typically regarding a marked stressful event.
- Withdrawal from society
- Inability to sleep and concentrating
Therapy/Counseling
- Lifestyle adjustments
- Support groups and social support

Conclusion
It is not a one-size-fits-all condition, and understanding the different types of depression is essential for effective treatment and support. Whether it’s the chronic nature of Persistent Depressive Disorder or the cyclical nature of Bipolar Disorder, each type requires tailored care. If you or someone you know is struggling with this, seeking professional help is the first step toward healing. Therapy, medication, and lifestyle changes can help manage symptoms and lead to a fulfilling life despite the challenges it may present.
